“It is one of the most common genetic disorders in the world, not the rare, exotic disease some think it is”, says Dr. Jacob Pendergrast about sickle cell disease.
It is estimated that around 1 in 20 human beings on the planet carry the gene that causes sickle cell disease. Being a carrier of the gene usually doesn’t affect people, but having two copies (a result of inheriting a copy of the gene from each parent) results in sickle cell disease, and in areas of the world without basic medical care, up to 90% of these children will die before the age of five.
“It’s a grand evolutionary bargain,” explains Pendergrast, “the sickle gene has evolved as a defense against the malaria parasite, carried by mosquitoes. One gene will give you some protection against severe forms of malaria, but two can prove fatal. If a couple, where each parent carries the gene, go on to have four children, statistically one will not inherit the gene, two will be carriers and therefore have some protection from malaria, and the fourth child will likely die. It shows just how devastating malaria has been that these odds ended up constituting a net benefit for humanity.”
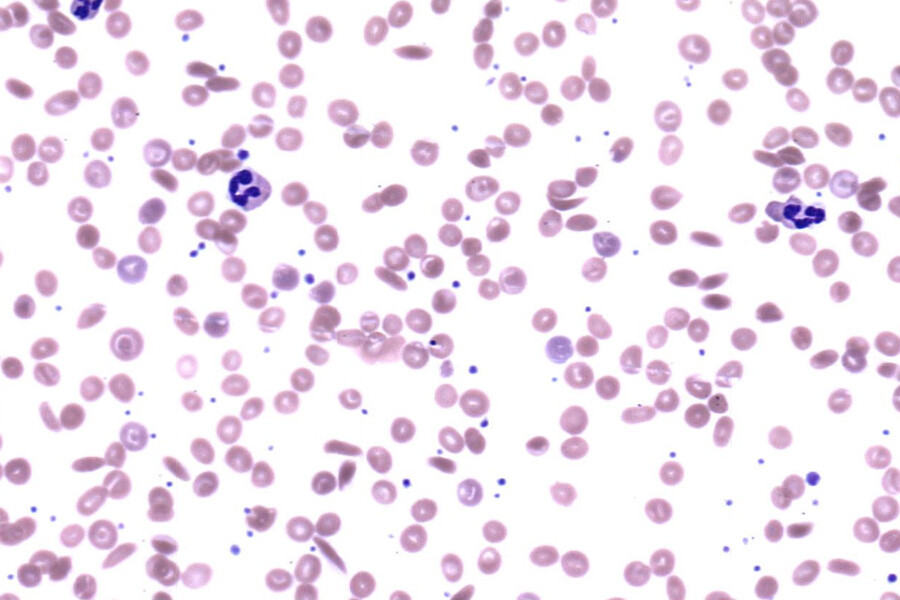
The gene for sickle cell disease likely emerged thousands of years ago, but the disease was only “discovered” by the Western medical system in 1910, and the responsible gene not identified until the 1950s. Progress in diagnostics and treatments has been relatively recent. Working at the forefront of evolving care and research into this disease, Pendergrast is an Associate Professor in the Department of Laboratory Medicine and Pathobiology in the Temerty Faculty of Medicine, and Medical Director of the University Health Network’s Blood Transfusion Service. His clinical practice in the Toronto General Hospital's Red Blood Cell Disorders Clinic is centred on the provision of blood products to patients with sickle cell disease, thalassemia and other related conditions. Pendergrast sometimes likens his clinic to “a refugee camp from the millennia-length war between humanity and malaria”.
“It is often seen as disease that only affects individuals in African countries, but that is a misconception. The prevalence is determined by historical exposure to malaria so, for example, there is very little sickle cell disease in Ethiopia (a more mountainous country with relatively few mosquitoes), while India has one of the largest populations of sickle cell patients in the world,” he explains.
In one of his studies, the prevalence of sickle cell disease assessed in Ontario was estimated to be 3 500 patients. While this still constitutes a rare disorder in a province of over 14 million, 30 to 40 babies are born here with disease each year and combined with the effects of immigration and lengthening life expectancy, the number affected is steadily growing. Moreover, the effects of international migration and population mixing means that a “genetic disease like this is not confined to any one racial group,” he says, which is one of the reasons all newborns in Ontario are now screened for sickle cell disease.
One of the challenges for people living with sickle cell disease is that for years it was primarily a pediatric condition, with an average life expectancy in North America not exceeding 18 years up until the 1970s. With advancements in diagnosis and treatment, patients can now be expected to live into their 60s or 70s, but the system hasn’t kept up. “Patients generally have good access to comprehensive care when they are young, but as soon as they hit 18 and leave their pediatric programs, many are left to drift from hospital to hospital, receiving only short-term, emergency care. At the Toronto General Hospital, we offer one of the few adult comprehensive sickle cell programs in Ontario so we can make a big impact, which is very rewarding.”
The disease can be an incredible burden to patients and their families, but also to the health systems and societies. It is estimated that there are over 100,000 people in the United States with sickle cell disease, with the lifetime healthcare costs for each person averaging $1 million. Much of that cost could be prevented through the broader use of inexpensive medications such as hydroxyurea and the judicious application of blood transfusion therapy. Even still, sickle cell disease has historically been neglected as a medical condition.
“A certain amount of intrinsic bias arising from the racialized nature of the disease has resulted in a chronic lack of funding and resources, meaning this common genetic disorder has received relatively little attention,” says Pendergrast. That, however, is now changing, particularly with the issuance of a new strategic plan by the US National Heart Lung and Blood Institute in 2008 which named sickle cell disease as one of its priority areas for research funding. This was followed by a surge of interest by both the academic world and the pharmaceutical industry in better understanding disease pathophysiology and developing novel therapeutics.
“It's an exciting time to study and treat sickle cell patients right now as treatment options are developing rapidly. Sickle cell was truly the first molecular disease, one in which all the many different clinical manifestations can be traced back to a single genetic variant that was first identified in the 1950s. It is in fact the perfect disease to treat with gene therapy because not only does it arise from a single mutation, but there is also a compensatory gene, the gamma-globin gene, present in every patient which if reactivated can effectively eliminate all signs and symptoms of the disease. The cure is within our patients already, it's just a matter of turning that gene back on again”.
With a network of highly motivated researchers, clinicians and laboratory physicians like Pendergrast being given new access to funding, including a promising trial of gene therapy set to start enrolling soon at the Princess Margaret Centre, there is hope for the future.
Find out more about the Hematological Pathology program and research in Hematopathology at LMP
This initiative showcases the following pillars of the LMP strategic plan: Impactful Research (pillar 3), and Disruptive Innovation (pillar 4)