Alumni focus: when cells in the cardiovascular system forget who they are
“I find cardiovascular disease so fascinating as you can look at the problems from so many angles. It’s a complex system where different factors interplay like physical forces with the blood flow, local microenvironments, the immune system, inflammation, and metabolism,” explains Dr. David Ngai, “but on a personal level, after my dad underwent bypass surgery when I was a kid, I wanted to understand how it all worked and why that happened to him.”
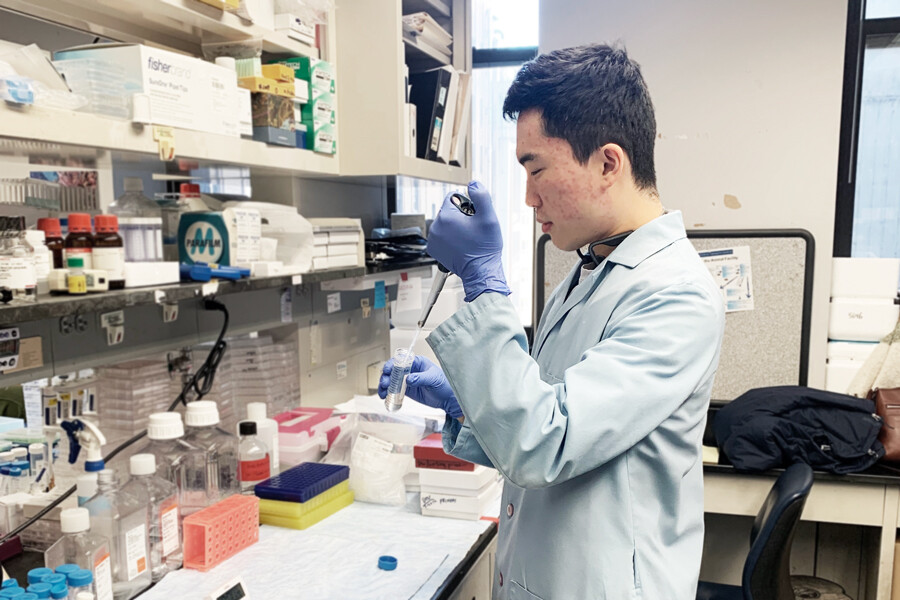
David, now a Post Doc in the lab of Dr. Ira Tabas at Columbia University in New York, started his journey into cardiovascular research in the Department of Laboratory Medicine and Pathobiology in the Temerty Faculty of Medicine and has now discovered the signaling pathways that cause cells in the cardiovascular system to forget their original function and start to calcify.
“I was really confused when I started my undergrad and wasn’t sure what I wanted to do,” laughs David, “I went into science and really thought I’d end up in medical school”. He heard about the Specialist Program in Pathobiology from fellow students when trying to decide what to study. He was initially daunted by how rigorous the program was but realized the classes covered many things he was interested in, particularly cardiovascular disease, so decided to apply and follow it with medical school.
Curious about research, David applied extensively for summer research placements during his program. Not knowing what he wanted to do made him open to trying many areas. His first placement was the Department of Molecular Genetics on bacterial evolution and antibiotic resistance, followed by studying new drugs for schizophrenia at the Centre for Addiction and Mental Health (CAMH). Neither experience was what he was looking for, so he went back to his initial inspiration and joined Dr. Warren Lee’s Lab in LMP looking at the effects of red meat consumption on cardiovascular health. “That really helped me realize that my interest lay in cardiovascular research”.
He applied to medical school in his fourth year, and while in Dr. Michelle Bendeck’s class ‘Pathobiology of the Cardiovascular System’ one day, he approached her for one final summer experience. “I was really too late to apply for a summer position, but I thought I’d ask so I just walked up to her at the end of class and the following week I was in her office discussing projects!” When medical school didn’t work out, he decided to stay in the Bendeck Lab for an MSc. While there he realized that he didn’t want to reapply for medical school and that a research career suited him better.
I think a lot of it was going with the flow. Most of the people around me planned on going to medical school so that just rubbed off on me. Once I was immersed in the research environment, I realized that was what I loved. I like the lifestyle and freedom research gives you – it’s challenging but allows for creativity.
A transfer exam later and he committed to a PhD instead.
David, without realizing it, was behaving like the structures and systems he studied in the Bendeck Lab. He started following the path to medical school because of the forces around him. In the lab he studied how the physical forces in the environment can sometimes cause cells to change their function.
Cells not only respond to the biochemical environment, for example the levels of cholesterol, but also the physical forces around them like the force of the blood flow. These forces contribute to the regulation of cardiovascular health and the functions of the cells. David was particularly interested in the elasticity and structure of arteries and how that environment affects cell function.
“The stiffness of the tissues gives cells, particularly the stem cells, cues that they’re a certain type of tissue. Once that tissue starts to harden due to disease it can give them the wrong signal and make them change their function,” he explains. Stiffening of the arteries results in vascular calcification – where the smooth muscle cells of the artery walls think they should be bone cells. This can happen in diabetics, those with certain kidney diseases, cardiovascular disease, or in aging populations. Once the arteries lose their elasticity, blood flow becomes hindered, the heart must work harder and can end up in heart failure.
David investigated how a membrane surface protein called DDR1 affected this process. Believed to have some mechano-sensing properties, it directly interacts with the environment it’s in.
“We discovered that DDR1 does have a significant role to play. When stiffening starts to occur, DDR1 drives up the signaling pathways which are normally found in the development of bone – mimicking bone development in the wrong type of cell. Once the tissue calcifies, more DDR1 is produced so it creates a feed-forward loop, the surroundings become even stiffer, and it exacerbates the problem”.
His research progressed to discovering how DDR1 controls its own expression using the YAP/TAZ stiffness sensing molecules: DDR1 signals for YAP/TAZ to create more DDR1 and the cycle continues. His work was recently published in Matrix Biology: Stiffness-responsive feedback autoregulation of DDR1 expression is mediated by a DDR1-YAP/TAZ axis.
Treatments for vascular calcification are still very limited. “We know how calcification happens, but this is the normal process for bone development, just in the wrong place. If we stop the process, we cause osteoporosis. There are so many signaling pathways in disease that overlap with normal cellular processes so it’s difficult to pinpoint specific treatment mechanisms that only target the diseased tissue and don't affect other parts of the body. It can have potential side effects that are worse than the disease itself”.
David is now expanding his cardiovascular research in the Tabas Lab by investigating efferocytosis: the process by which immune cells clear out dead cells in the body to prevent a chronic inflammatory response. When immune cells digest these cells, they not only prevent a buildup in the body and consequent inflammation but release amino acids and other useful elements into the system which helps the body heal. “I’m fascinated by this whole process and how we could potentially harness it to regress atherosclerotic plaques.”
Being part of LMP certainly influenced the way David thinks. “There is such a breadth of research going on in LMP. You get more ideas from listening to people speak about other fields rather than only listening to your own. That was what helped develop my scientific thinking”.