Undergraduate conference shows laboratory medicine’s role in understanding, diagnosing and treating COVID-19
On Saturday January 9th, 2021, the Laboratory Medicine & Pathobiology Student Union (LMPSU) in the Temerty Faculty of Medicine, University of Toronto, held its 9th annual research conference: COVID-19: Investigating a viral phenomenon.
Nearly 700 registered to attend the virtual conference to hear about some of the latest developments in COVID-19 laboratory medicine. Many were undergraduate students at the University of Toronto, but undergraduates from universities across Canada, graduate students and health professionals also joined the discussions.
Presentations by a range of researchers demonstrated the incredible progress made in the fight against COVID-19 and, although it is clear more needs to be done, it left attendees with hope for the future.
Isolating the virus and understanding COVID-19
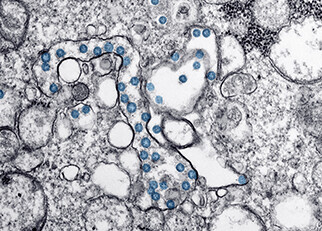
Keynote speakers Dr. Samira Mubareka and Dr. Robert Kozak, both in the Department of Laboratory Medicine & Pathobiology in the Temerty Faculty of Medicine, kicked off the day discussing how they isolated SARS-CoV-2 (the virus that causes COVID-19) in the Lab.
Dr. Mubareka covered several projects her students were involved in, from isolating and sequencing the virus, to using a breathing mannequin, affectionally nicknamed Quarantino, to study how the virus spread.
The research team set up a simulated ICU and investigated how the virus could disperse under various methods of patient ventilation. Read more from Ryan Hiebert, a member of the research group in Completing a Masters in infectious disease during COVID-19: making a difference for frontline healthcare workers.
She emphasised how a virus can mutate once or twice a month and the importance of vigilance with this virus, combining genomics and epidemiology simultaneously.
Dr. Kozak described how Nasopharyngeal swabs (PCR tests) are most effective, but can be difficult to administer, and presented the work he was involved in evaluating the sensitivity and specificity of saliva tests. He also reviewed his work on the efficacy of interferon in the treatment of COVID-19.
Studying populations in Canada and India
Dr. Prabhat Jha, the University of Toronto Endowed Professor in Global Health and Epidemiology at the Dalla Lana School of Public Health, talked about a study he designed (the Ab-C study) with the help of the polling company, Angus Reid Forum.
They surveyed 19,000 Canadians and took blood samples to monitor the prevalence of COVID-19 in the population and is doing another follow-up shortly.
With their data they have developed a mortality prediction model to try and predict future infection and mortality rates, though studies need to be ongoing.
Diagnostic tools for lower-income countries
Dr. Keith Pardee, Canada Research Chair in Synthetic Biology in Human Health and Assistant Professor in the Leslie Dan Faculty of Pharmacy, discussed an emerging role for synthetic biology and low-cost hardware to develop diagnostic tests suitable to use in underdeveloped countries, or areas with remote populations.
He and his group have developed a paper-based sensor system using portable readers: the “lab-in-a-box”. Initially developed in response to the Zika virus, the team has adapted it for use in COVID-19 detection. This diagnostic tool is now being tested in Latin America.
Treatments for COVID-19
The rest of the day was dedicated to discussing various treatment methods for COVID-19.
Dr. Michael Joyner, Mayo Clinic Professor of Anesthesiology, and Dr. Jeannie Callum, from LMP, both discussed different aspects of using Convalescent Plasma (the transfer of antibodies from a recovering patient) for COVID-19. A method, used successfully for SARS and measles, has had promising results in COVID patients when used early and clinical trials are still underway.
Dr. Eleanor Fish, Department of Immunology, covered the use of interferons in treatment. Interferons are proteins that are part of your natural defenses and trigger your immune response. Viruses can block natural interferons so using more in therapies can help. She and her collaborators have had encouraging results in patients with COVID who showed decreased viral shedding with this treatment.
Dr. Aled Edwards, Professor of Medical Genetics and Medical Biophysics, closed the conference with a stimulating talk on the importance of open research and how sharing results with the scientific community can facilitate research, the understanding of disease, and the development of new treatments.
A broad view of how laboratory medicine is fighting COVID-19
The wide range of topics showed the audience the variety of roles laboratory medicine can play in a pandemic.
Organiser, and Co-president of the Laboratory Medicine & Pathobiology Student Union (LMPSU), Ziqi Liu commented, “The conference has been incredible. The whole team has been proud to showcase such a range of powerful research.”
“It really inspired many of those attending, particularly those of us at the start of our research careers,” added co-president Karen Mao, “To see what is possible in laboratory medicine and the myriad of ways it can play a role in directly affecting patient outcomes, and all our lives.”
“What’s really been great today has been to share that feeling of hope,” continued Ziqi, ”Science will find a way - developments and progress is happening at such a rapid rate and I’m very proud to feel a part of it here, at the University of Toronto.”
With thanks to Britney Tian and Nathan Vo for taking detailed notes at the conference.



