Main Second Level Navigation
Dec 13, 2023
Unraveling the enigma of Nodding Syndrome
Programs: Graduate, Agile education, Research: Brain & Neuroscience, Inclusive community

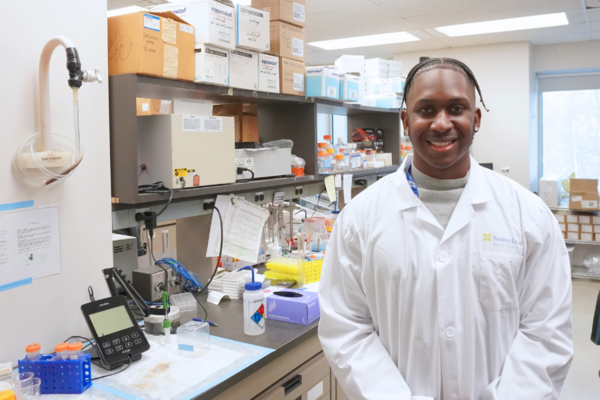
Kenneth Kodja
The team in Uganda (from left to right): Dr. Sylvester Onzivua, Dr. Michael Pollanen, Joe Otto, MSc student Kenneth Kodja, George Otto