How the COVID-19 pandemic impacted the next generation of scientists

The first confirmed COVID-19 case in Canada was reported on January 25, 2020, at Sunnybrook Health Centre. Scientists in the Department of Laboratory Medicine immediately began to investigate the SARS-CoV-2 pathogen and the team based at Sunnybrook, including Dr. Samira Mubareka and Dr. Rob Kozak, were among the first to isolate the virus. This allowed others to study and understand the disease. On March 11, 2020, the World Health Organisation (WHO) officially declared COVID-19 a pandemic.
Scientists in LMP rose to the challenges the world faced with this new and deadly virus. From vaccine development, to mask testing, to understanding how the disease spread and affected various parts of the body, LMP was at the forefront of knowledge building, while our trainees and clinicians stepped up to care for patients and vaccinate individuals.
The next three years not only affected lives, public health, and societies at large but had a huge impact on many students and trainees in LMP, often changing the course of their studies and how they saw their place in the world. The pandemic showed many young scientists the difference their work could make to people’s health, in real-time, how to adapt, and how to translate skill sets to different areas.

Yaejin Lee, now in her 2nd year of a PhD with Dr. Samira Mubareka (Sunnybrook Health Science Centre) and Dr. Allison McGeer (Mount Sinai Hospital) was studying respiratory viruses, so a shift to studying the transmission of SARS-CoV-2 was a natural one. She is currently investigating the characterization of Omicron sub-lineages to understand the evolving intrinsic viral properties associated with enhanced transmission.
“Since I was young, my heart was set on pursuing a career within the field of infectious diseases. I grew up in Zimbabwe and experienced how infectious diseases could negatively affect the community. During my undergrad, I had opportunities to be trained in labs studying respiratory viruses and further realized my dedication to pursue research to create an impact on the community. So, I was thrilled to study the novel coronavirus, especially within the containment level 3 which is a rare opportunity offered to trainees.”

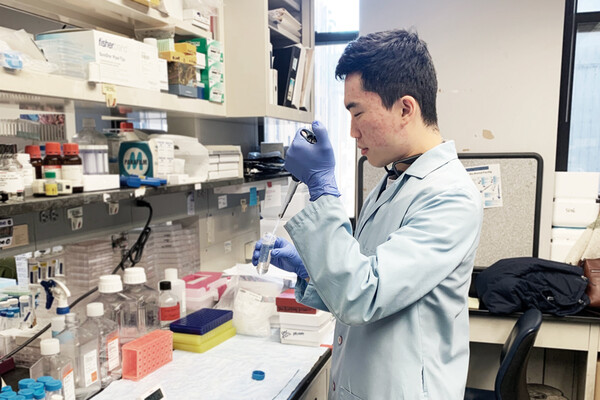
For trainees such as Peter Zhou, the pandemic reinforced how he saw his role in the world, “The pandemic has caused widespread cases and death worldwide and overwhelmed healthcare systems in many countries. As a medical researcher, I felt it was a chance and responsibility to apply my knowledge to help”.
Peter was in the final stages of his PhD with Dr. Jim Hu at SickKids when the pandemic was declared. He switched to studying vaccines which he is now pursuing in further studies. “Studying COVID-19 vaccines required me to transition from gene editing to immunology. I spent a lot of time reading and absorbing new immunological knowledge. I also had to complete several months of training to be able to do SARS-CoV-2 work in the containment level-3 lab at U of T”.
Now pursuing post-Doctoral studies in Dr. Jun Liu’s lab (Department of Molecular Genetics) his research is helping to develop nasal vaccines. “Current parenteral vaccines are administrated by intramuscular route, which induces potent systemic immunity but limited airway mucosal immunity. Since SARS-CoV-2 is mainly transmitted through the respiratory route, intranasal delivery of a mucosal vaccine has the potential of inducing strong mucosal immunity to prevent viral entry and transmission”, he explained.

Dakota Gustafson was completing his PhD in the lab of Dr. Jason Fish. His research was dedicated to exploring the clinical utility of novel cardiovascular biomarkers, with a particular focus on those related to endothelial function. He was curious about how these biomarkers might complement our current diagnostic tools and help gain a more comprehensive understanding of cardiovascular disease.
“Like many others, I hadn't originally planned on pursuing research related to COVID-19. However, the gravity of the pandemic and its profound impact on global health and society compelled the lab to collectively shift focus and contribute to the ongoing efforts to combat the virus”.
The Fish Lab recognized the urgent need to better understand the impact of COVID-19 on the cardiovascular system and to develop more effective strategies for diagnosing and treating these complications. “Dr. Fish and Dr. Kathryn Howe recognized early on how our existing research could be applied to the global fight against COVID-19. Their vision and leadership inspired us to pivot our research focus, develop some amazing collaborations and make meaningful contributions towards the effort of combating the virus,” said Gustafson.
Gustafson found that one of the greatest lessons he learned was how to adapt, “In research, we are constantly confronted with unexpected obstacles and setbacks that are inherent to the discovery process. Learning to translate our skillsets across different areas (such as moving an entire research focus to COVID-19) or adjusting our methods in creative ways can be challenging, yet it is essential to the research process and can lead to exciting new findings”.
The unique experience of the pandemic and being able to see research translated at high speed, made many trainees truly understand the impact their work could make in the world. For Gustafson, that means seeing the bigger picture. He is now doing an MD-MSc in Epidemiology at Queen's University, where he is investigating the incidence of mental illness in cardiac arrest survivors. “Looking ahead, my goal is to merge my skillsets and develop a truly translational approach to problem-solving, one that can address issues on both a microscopic and macroscopic scale”.