U of T researchers seek to understand the novel coronavirus on a 'deep molecular level'

SARS-CoV-2 has shut down the world by spreading furiously from one person to another. Now scientists want to trace its steps within cells to stop it.
Supported by the Toronto COVID-19 Action Fund, researchers from across the University of Toronto and its hospital partners, as well as McMaster University, have joined forces to identify all components of the human cellular machinery involved in the life cycle of SARS-CoV-2.
Led by Jason Moffat, a professor of molecular genetics in the Temerty Faculty of Medicine and at the Donnelly Centre for Cellular and Biomolecular Research, the team will apply CRISPR – a gene engineering tool that uses a sequence of DNA and its associated protein to edit the base pairs of a gene – to pinpoint all gene-encoded protein factors in human cells exploited by the virus to get inside and multiply.
The hope is that there are already clinically approved drugs that target some of these factors that could be quickly repurposed for COVID-19.
“We want to understand the host factors required for the life cycle of the virus on a very deep molecular level,” says Moffat. “Our goal is to see if we can repurpose any drugs in a rational way after we understand more about what the host factors are doing.”
He added that it is also important to understand the biology of the virus.
“Funding basic science is critical for understanding how to manage new biological threats like COVID-19,” says Moffat. “Had there been more opportunities for researchers to break down what the SARS virus was doing following the outbreak in 2003, we probably would have been in a much better position to manage the current pandemic.”
Like all viruses, SARS-CoV-2 hijacks host molecular machinery for its own ends. It is now established that the virus gains entry by binding the ACE2 receptor with help from another human enzyme known as TMPRSS2. But there are certainly many more factors involved at various stages of its life cycle.
“We often think of viruses as simple – they introduce their genome into the host cell and replicate themselves to release more virus,” says Moffat’s co-investigator Scott Gray-Owen, a professor of molecular genetics in U of T’s Faculty of Medicine who studies infection and the body’s response to it.
“But for any pathogen to cause infection in a host, it has to overcome many different aspects of the immune response. Our aim is therefore to find creative ways to intervene in how the virus replicates or evades immunity so as to stop its spread and halt the progression of disease.”
The researchers are casting a wide net to find all host factors involved with the novel coronavirus. With CRISPR, they will switch off every gene in human cells infected with SARS-CoV-2. If a gene is essential for the virus, then turning it off will allow those cells to resist the infection while the rest will die.
These experiments will be done in the Faculty of Medicine’s Containment Level 3 (CL3) lab, which is directed by Gray-Owen and supports research with all but the highest risk-level pathogens. The lab is required for work with SARS-CoV-2, which has a risk group rating of three.
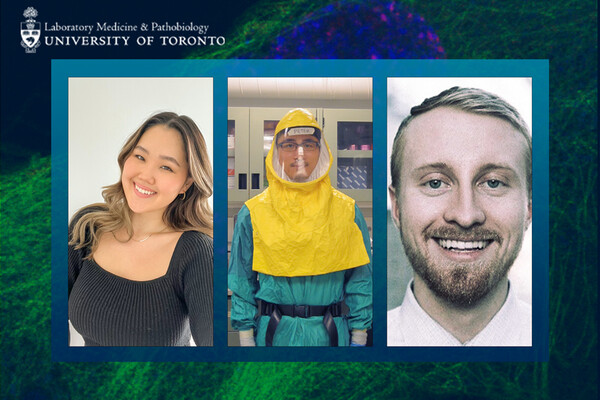
The research is being spearheaded by Katie Chan and Furkan Guvenc, a senior research associate and a graduate student in Moffat and Gray-Owen’s labs, respectively. To stay safe while handling the virus, they will wear full-body protection suits equipped with air purification systems.
“Once you put on the suit, you don’t want to come out,” says Guvenc, who previously studied HIV, also a risk group three pathogen, and is accustomed to going without food, drink or bathroom breaks for an entire day. “It’s a very ascetic exercise. You perform the experiments until they are done, however long that may be,” he says.
Also on the team are Samira Mubareka, of the SunnyBrook Health Sciences Centre and U of T’s department of Laboratory Medicine and Pathobiology in the Temerty Faculty, and Karen Mossman, a professor of pathology and molecular medicine at McMaster University. Mubareka and Mossman were among the first in Canada to isolate SARS-CoV-2 from patient samples and are providing the live virus for the experiments.
As well, University Professor Jack Greenblatt and Professor Benjamin Blencowe, both of the Donnelly Centre, will study how gene expression changes in response to infection for more clues about how COVID-19 develops at the cellular level.
And Mikko Taipale, an assistant professor of molecular genetics in the Donnelly Centre, and Shana Kelley, University Professor at the Leslie Dan Faculty of Pharmacy, will identify the factors required for the production and maintenance of the ACE2 receptor on the cell surface.
Moffat expects that they will have a list of key host factors by July.
“If we could find a molecular pathway that is essential for the virus and there is a clinically viable drug, then this could have a rapid impact on intervention,” says Moffat.
“But the overall knowledge we’ll gain might also help us confront other coronaviruses in the future.”